Table of Contents
A
Ablation
Cardiac ablation is a surgical procedure to treat arrhythmias. A catheter is inserted through a vein in the groin area and is conducted up to the heart. This flexible catheter has an electrode at the top that emits heat and cauterizes the abnormal electrical pathway.
Adenosine
Adenosine is a drug administered intravenously on patients with SVT for termination of an episode.
Atria
Atria represent two of the four chambers of the heart, situated above the ventricles.
Atrioventricular Node (AV)
The AV node lies on the right side of the partition that divides the atria, near the bottom of the right atrium. It is called a gatekeeper for the ventricles because it collects all the impulses from the atria.
When the impulses from the sinoatrial node (SA) reach the atrioventricular node (AV), they are delayed for about a tenth of a second. This plays a critical function in allowing atria to contract and empty their contents into ventricles before ventricular contractions.
Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
AVNRT is the most common type of supraventricular tachycardia, occurring in approximately 60% of patients.
In atrioventricular nodal re-entrant tachycardia (AVNRT), the aberrant loop of electricity originates around the AV node above the Bundle of His. This impulse doesn’t die out at the end of one cardiac cycle but tends to create a circular signal around the node rather than simply passing it along as it ought to do. Imagine a racing car going round and round in a circular motion around a race track.
This aberrant circuit is created by forming two pathways, both located within the AV node that is the slow pathway and the fast pathway.
The usual pathway that leads the impulse from the atria through the atrioventricular node (AV) to the ventricles is the fast pathway.
That is, AVNRT happens when a premature impulse arrives at the AV node, and the fast pathway is non-excitable or not in the position to accept the impulse and the slow path is ready or excitable. The slow pathway conducts the impulse and can activate the fast pathway and send a signal back up, which will again trigger the slow pathway, sending the impulse down to the ventricles faster than usual, up to 250 beats per minute. This will continue until the circuit is interrupted with one of the medical maneuvers or stopped by itself.
The slow pathway is usually the one that will be ablated if the person chooses to undergo ablation.
Atrioventricular Reentrant Tachycardia (AVRT)
This form of arrhythmia is the second most commonly occurring in approximately 30% of patients presenting with supraventricular tachycardia. It affects a population younger than those affected by AVRT with a slight male predominance at a ratio of 2:1 against the female population. Like the AVNRT, most patients suffering from the condition have no underlying structural defects. However, several studies have reported a link between the condition and Ebstein’s anomaly, rare congenital heart disease in certain patients.
AVRT occasionally occurs together with Wolff-Parkinson-White syndrome posing a risk for the development of atrial fibrillation and atrial flutter in these patients. Therefore, this is a diagnosis that should not be missed. It can be pointed out through findings on an ECG such as a delta wave.
The symptoms of AVRT are of the same kind as that of any other SVT. They comprise palpitations, shortness of breath, diminished exercise tolerance, fatigue, chest discomfort, dizziness, lightheadedness, and weakness.
How does the electrical impulse travel in Atrioventricular Reentrant Tachycardia (AVRT)?
AVRT is when the abnormal electrical impulse goes in a circular motion between two pathways.
In a normal heart, only a single conduction pathway exists from the sinoatrial node to the bundle of His.
People with AVRT are born with this extra anatomical pathway called the bundle of Kent. It is an abnormal circuit.
However, in AVRT, there are two pathways – one pathway is the normal AV conduction pathway, and the second pathway is the abnormal connection you have been born with, located somewhere between atria and ventricles.
The electrical impulse usually can go from the atrium through the AV node to the ventricles and the bundle of His and right and left Purkinje fibers causing ventricular stimulation and contraction, then dies out and the sinoatrial node (SA) is prepared for releasing another impulse.
When an extra bypass pathway is present that connects the atrium with the ventricle, there is an aberrant loop of electric current that doesn’t cease after ventricular contraction but goes back to back between the two pathways.
In AVRT, the signal travels down the heart either the normal pathway or the accessory pathway and returns via the other. What usually happens in AVRT is that the impulse travels down along the normal cardiac conducting system to the ventricles. Instead of dying out, it will travel back along the accessory pathway, and then the re-entrant circuit occurs. Re-entering the atria, the signal loops back to the atrioventricular node (AV). Instead of the impulse initiating from the sinoatrial node (SA), it begins in the atria and goes to the ventricles and Purkinje fibers again. It will follow this track on and on.
C
Cardiac Conduction System
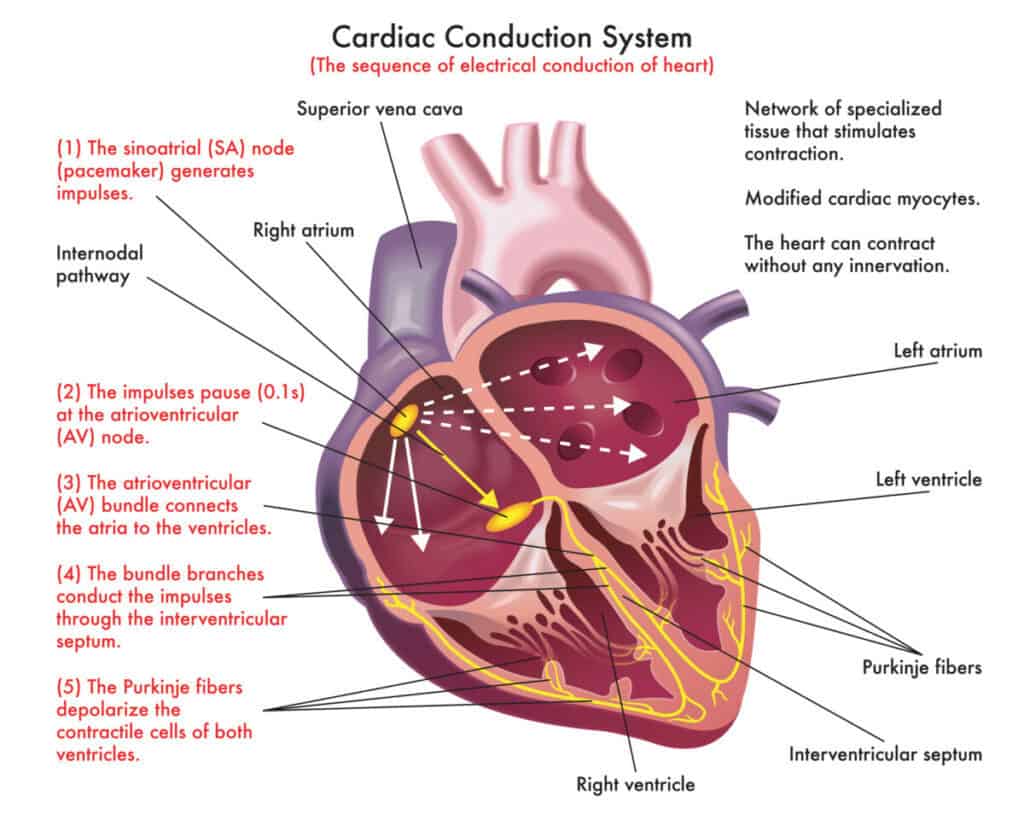
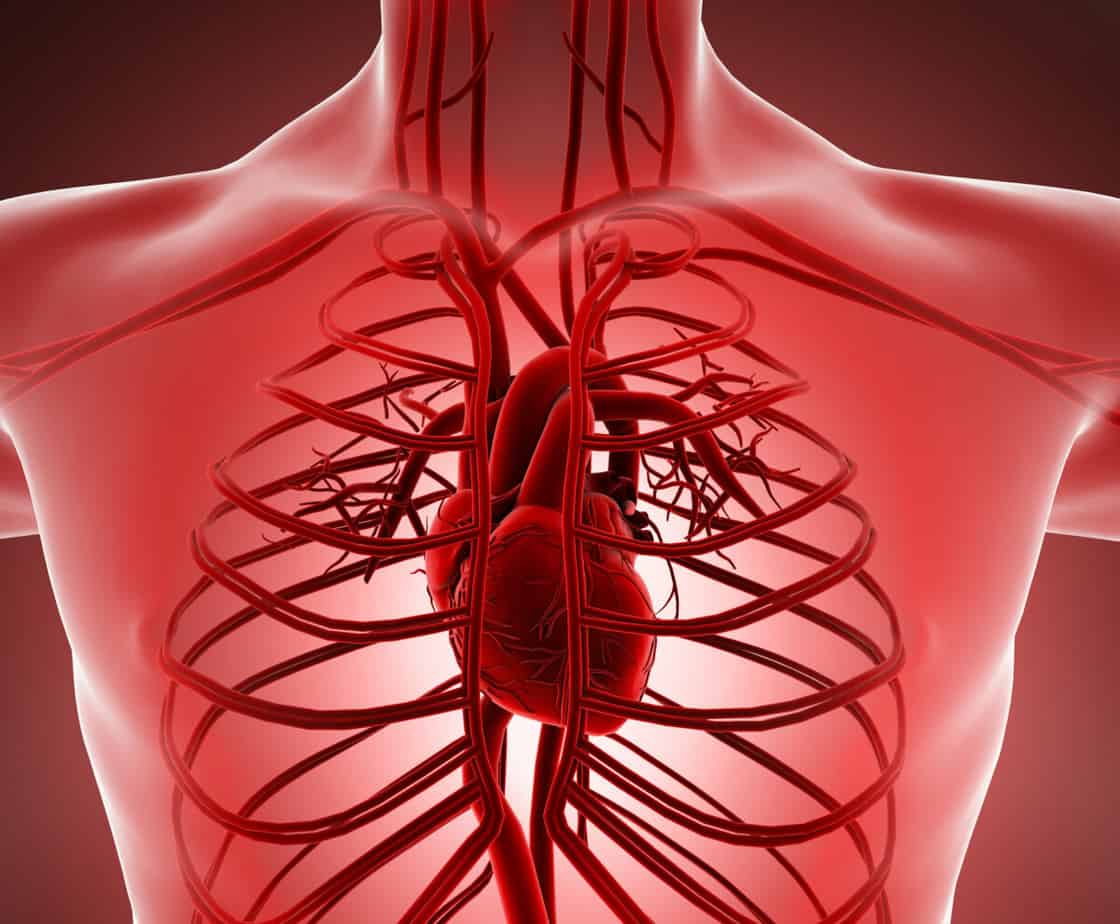
The cardiac conduction system is also known as the electrical system of the heart. Electricity is the driving force behind every heartbeat. Our heart needs electricity to work.
This mechanism represents the built-in electrical system placed in the heart walls that allows the electricity to be generated and coordinates the rhythm and heart movement pattern.
The electrical pathway of the heart consists of:
- Sinoatrial node (SA)
- Atrioventricular node (NA)
- Atrioventricular bundle or bundle of HIS
- Bundle branches
- Purkinje fibers
E
Echocardiogram
Echocardiogram is a non-invasive investigation. It uses sound reflection (echo) to examine the structure of the heart.
Electrocardiogram (ECG)
The electrocardiogram (ECG) is the first tool necessary to diagnose supraventricular tachycardia (SVT). It is a painless, quick, noninvasive test that measures the heart’s electrical activity, including the timing and duration of each electrical phase in a heartbeat.
The ECG does not directly measure the pulse, but the heart’s electrical impulse in one heartbeat.
With each beat, an electrical impulse (or “wave”) moves through the heart. This wave produces a muscle contraction that contributes to pump blood from the heart to a different body part.
A heartbeat on ECG will show the timing of the top and lower chambers.
The right and left atria make the first wave called a “P” wave – following a flat line when the electrical impulse travels to the bottom of the chambers.
The ventricles make the next wave called a “QRS complex.”
The final wave or “T wave” represents electrical recovery to a resting state for the ventricles.
How is it done?
The patient lies on a bed, and electrodes are placed on the chest, arms, and legs—the electrodes record only electricity that travels naturally through the heart. The electricity does not pass from the pads to the patient. The patient will be asked to lie entirely for several minutes while resting–heart activity is measured and recorded.
The standard ECG has about 12 leads and ten electrodes. Note that leads are not the same as electrodes technically, but they are used interchangeably at times. The electrodes in contact with the patient’s body are 10 in number, and they are connected to the 12 leads. See leads more like a measuring system while electrodes are the physical wires.
Four of the leads are placed on both arms and legs, and the other six leads are placed on measured intervals from the sternum to the left chest. The leads have to be placed correctly, or the readings may be wrong.
The tracing of the electrical activity of the heart is recorded and printed on a moving paper for the proper analysis by the specialist. It can also appear as a moving line on the screen. There is no pain or risk associated with this test. It can appear some minor discomfort when the stickers are removed.
What can we find out from the EKG?
The ECG looks for conduction and rhythm abnormalities and can also give information about the heart’s anatomy by inference. It could detect if you have narrowed coronary arteries due to fatty deposits if you had any previous heart attack or enlargement of the heart.
If the patient is experiencing SVT (Supraventricular tachycardia) during the EKG, this affection’s diagnosis can be clear.
SVT will present as abnormal PQRST readings. More attention is paid to the QRS and ST waves, though.
Ectopic Heartbeats
Ectopic is the early or additional heartbeat that leads to the perception of a missed beat. Ectopic means misplaced or in an abnormal place. They are the early or additional heartbeat that can lead to the perception of palpitations.
Ectopic beats are premature beats that can be picked up on ECG. Their origin could be traced from any location in the heart.
What happens in the heart when we get an ectopic?
When an ectopic arises, we have the following sequence: normal beat – ectopic – normal beat.
A healthy heart is working rhythmically as it normally should do, beat after beat after beat. Still, it comes a time when some cells from your heart, others than those from the sinoatrial node (SA), get irritated by your intake of coffee or your increasing stress and get fired, releasing an early impulse between two normal beats. This is an ectopic or an extra beat.
This ectopic is not so strong to be perceived like a beat. It is weak, so it felt like a pause, causing the patient to say that the heart has stopped for a while but can create an inadequate heart contraction. Because the contraction is weak, it doesn’t pump all the blood out of the heart. There is likely to be a more extended time between the ectopic and the next normal beat than between two normal beats.
Therefore, we have some blood accumulating in the ventricles from the ectopic beat and the blood coming in the ventricles from the next normal beat. This makes the normal beat that follows the ectopic to be much stronger, and sometimes chest pain is present because the ventricles are filled with more blood than usual and need greater force to contract and eject all that blood in the circulation.
H
Heartbeat
Heartbeats are forceful compressions that ensure that blood circulates the body.
In one heartbeat, the impulse travels throughout the heart along the cardiac conduction system’s components to produce the heart’s contraction responsible for pumping the blood. Then, the impulse dies out.
In a normal single heartbeat, one electrical impulse is generated in the sinoatrial node (SA). The electricity passes then through both atrium to the atrioventricular node (AV). The impulse travels further down to the ventricles along with the bundle of His and right and left Purkinje fibers.
Holter Monitor
An ECG records the electrical activity of the heart for only a few seconds.
A Holter monitor is a 24-hour portable ECG used to record the heart rhythm continuously during day-to-day activities.
You are going to have electrodes placed on your chest, which are attached to a small device. The device can be attached to a belt around the waist or placed in a pocket.
During Holter monitoring, a journal will be kept, in which the patient is asked to note all the activities, medications, or symptoms that occurred while wearing the device. Later on, they are compared with the information recorded on the monitor.
A Holter monitor can detect any abnormal heart rhythm.
O
Oxygen Saturation
Oxygen saturation shows the level of oxygen, reaching cells and organs throughout the body. A healthy value is above 95%. A value lower than 95% means that the body will suffer and no longer function at its optimal level.
P
Premature Atrial Contractions (PAC)
Premature Atrial Contractions (PACs) – Most frequent form of arrhythmia occurs due to an early release of an electrical impulse in the upper chambers of the heart called the atria that leads to a premature contraction. It is quite a normal occurrence. Though palpitations are commonly reported as symptoms, many patients perceive them as a missed or skipped heartbeat.
Premature Ventricular Contractions (PVC)
Premature ventricular contraction (PVC) – They occur when the early impulses arise in the lower chambers of the heart called ventricles. On ECG it is noted as bizarre-shaped (wide) QRS complexes.
Pulse
The heart’s pumping action into the arteries occurs rhythmically and repeatedly gives rise to tactile arterial palpation felt with fingertips’ help over the major arteries. The pulse can be felt manually in places where the artery can be compressed over a hard platform such as:
• at the neck (carotid artery),
• wrist (radial artery),
• at the groin (femoral artery),
• behind the knee (popliteal artery),
• near the ankle (posterior tibial artery) and
• top or inner side of the foot (dorsalis pedis artery).
Normal pulse or heart rate at rest ranges from 60 to 100 beats per minute.
S
Syncope
It is often referred to as fainting or “passing out.” It is viewed as a transient loss of consciousness due to reduced blood flow to the brain.
Sinoatrial node (AV node)
AV node is the heart’s natural pacemaker, which sets the heart rate. The heart electrical impulses are generated from there, spreading throughout the heart and causing the heart to beat rhythmically.
Supraventricular tachycardia or SVT
Supraventricular tachycardia is a type of arrhythmia characterized by a rapid heart rate above 100 beats per minute from abnormal electrical activity in the atria, the heart’s top chambers.
Supraventricular simply means above ventricles, which indicates that the abnormal electrical activity occurs above ventricles in the atria.
It is a relatively common condition affecting people of all ages, including those without any preexisting heart conditions.
It is the most common form of abnormal rhythms of the heart in newborns and infants, affecting 1 in every 2500 children.
It is more common in people below 65 years, and the specialists say it is not life-threatening.
Most arrhythmias are benign or harmless, and the symptoms comprise of being barely perceptible to the cardiovascular system.
However, certain long-standing and severe arrhythmias require prompt treatment as they lead to inadequate blood supply to the body’s parts.
Stress Test
The stress test is an investigation used to assess how the heart performs, especially in relation to exercise.
It is usually done by making the patient exercise on a treadmill or ergometer that gradually puts the heart to work more and more.
The heart’s role is to continuously pump nutrient-rich and oxygenated blood throughout the body to the muscles and organs.
To do that, the heart must be permanently irrigated with oxygenated blood, which is done within the coronary arteries.
When fat deposits narrow one or more portions of the coronary arteries, the blood flow to the heart is restricted, and the heart does not get enough oxygen due to lack of blood supply.
This is called ischemia.
If the blood vessel is blocked at a rate of 70% or more, the person may experience symptoms as angina (pain in the chest, pressure, or heaviness).
When the muscles are put under stress by exercise, they will need more oxygen, but because the arteries are narrowed, less blood irrigates the heart and less oxygen.
This investigation allows the cardiologist to track the changes that appear on the electrocardiogram, blood pressure, and pulse during the effort of the patient and find out if the coronary ischemia( narrowing of coronary arteries) is present or not.
How is the stress test done?
The doctor will check if there are symptoms such as chest discomfort or fatigue before the test. Also, a resting ECG is performed.
Six to twelve electrodes are applied on the body, which are connected to an ECG device that monitors the electrical activity of the heart during the test.
A cuff for measuring blood pressure will be applied to the arm as well.
The patient is running on a treadmill for about 9-10 minutes, and every 3 minutes, the treadmill gets steeper and faster. The goal is to put the patient to a progressively increasing physical effort under permanent monitoring of the electrocardiogram, blood pressure, and sometimes other parameters such as oxygen saturation of the blood.
The test is stopped in the following situations:
- when the patient experiences symptoms like chest pain, difficulty in breathing, dizziness
- when there is an excessive increase in blood pressure, heart rate
- when ECG recording shows significant changes suggestive of myocardial ischemia
- when the patient has a low level of fitness and cannot cope with the increased effort despite the absence of ECG changes or suggestive symptoms
- when reaching a threshold of 85-90% of the patient’s target heart rate without abnormal ECG modifications. It is considered that the patient has a normal functional capacity.
Suppose a person experiences medical problems like arthritis, which might prevent them from doing proper exercise during the stress test. In that case, an alternative to this is pharmacological stress testing, where drugs are used to speed up the heartbeat instead of exercise.
What can we find out from the stress test?
An effort test measures how exercise influences blood pressure, heart rate, and the heart’s electrical activity. Some arrhythmias can be triggered or worsened by exercise and a stress test can determine if intense physical activity is the cause of your abnormal heart rhythm.
Other arrhythmias can be triggered by coronary artery disease, so your doctor wants to see if you show any symptoms of it.
The test detects coronary artery disease, but only if the arteries are narrowed in a 70% or greater proportion by observing the manifested symptoms. In coronary artery disease, the symptoms do not occur at rest but happen when the heart is forced to work hard and pump blood faster. Narrow arteries cannot provide enough blood to the heart. As a result, the patient experiences chest pain known in medical terms as angina.
When one or more arteries are blocked 70% or greater, there is a risk of a heart attack.
However, it is possible that a smaller blockage of less than 70%, which is not found in a stress test, forms clots in the arteries and can partially or entirely block the artery causing a heart attack.
A stress test is not 100% precise. Sometimes, it may indicate coronary heart disease in patients who do not have the condition. It is used more like a prognostic test.
T
Tilt Table Test
What is the Tilt Table Test?
Tilt table test is a form of a test where you are fastened to the table and it is brought in an almost upright position to evaluate your to investigate excessive fainting, otherwise called syncope in an individual.
The major reason for a test like this is to recreate the event of fainting; this is done using an electrocardiogram ECG recording and a blood pressure monitoring device. It is a kind of confirmatory test on an affected individual to diagnose the generic fainting or vasovagal fainting.
Fainting or syncope can occur due to shortage of nutrients or substrate supply to the human brain (oxygen and glucose). At times, heart problems can be a cause of fainting, like reduced heart rate that goes below 40 beats per minute or increased heart rate above the region of 140 beats per minute.
How can you prepare for the tilt table test?
You are likely asked to stay without food or any form of drink for up to six hours before the commencement of the test. Medications can go on normally except you are advised otherwise by your physician. It is always advisable that you prepare a transport for yourself to go back home because of the nature of the test.
Your healthcare provider will do the following before the commencement of the test:
• Some electrodes are placed on you in the chest, arm and leg region. These electrodes are connected to wires that connect to an electrocardiogram device that takes record of the heart rate.
• The connection of a device that records and monitor blood pressure to a finger or the arm, and sometimes it could be placed on both.
• Sometimes, in the second phase of the test, there may be a need to inject an intravenous line into a vein in the hand or the arm.
How is the tilt table test carried out?
• The test table is placed in a horizontal position, the devices connected to the individual (ECG and blood pressure) are set at minute zero.
• The table is then adjusted to a position of 75 to 80 degrees in the horizontal direction. The ECG and the blood pressure of the individual are taken into record at every minute in the space of thirty minutes.
• If there is any fainting experience from the patient, the ECG and blood pressure at that point is taken, and the test is halted by returning the table to its original horizontal position.
• When a patient does not experience fainting in the space of thirty minutes, the need to give the patient a form of nitroglycerin spray through the mouth arises. The test is restarted for the next fifteen minutes less should there be an issue of fainting.
The test is termed negative at the end of 45 minutes when there are no fainting issues experienced by the individual.
However, a positive test is recorded when there are issues of fainting experienced by the individual or when there is a reduction in the heart rate or blood pressure of the patient, also if the symptom recedes, when the table is adjusted back to normal.
Isoproterenol, which increases the heart rate, or sublingual nitroglycerine, which triggers a vasovagal response, is administered to the patient to provoke syncope symptoms when there is no visible sign of fainting during the first phase of the test, which lasts for 30 minutes.
What can we find out from the tilt table test?
The test can be either negative, typical when you didn’t faint during the test and had no other symptoms like dizziness and low blood pressure, or positive when your blood pressure was low during the test and experienced light-headed or fainting, the test is positive, abnormal.
The test is meant to find out the nature of the syncope according to different values of blood pressure and heart rate during the test.
It will determine if the syncope is a reflex/ neurally mediated syncope or a cardiac syncope.
V
Valsalva Maenouvre
Valsalva Maneuver is best done in a supine position (lying down) for people with supraventricular tachycardia to maximize pressure in the chest. Still, some people may be asked to sit, depending on the situation.
The patient will then be asked to forcibly exhale against a closed mouth and nose for 15 seconds or more.
In order to get more pressure to the chest, you will need to breathe out forcibly and contract your abdomen as if you are trying to empty your bowels.
This will increase pressure to the chest and also to a blood vessel called the thoracic aorta.
The thoracic aorta has a pressure point more accurately known as a baroreceptor. When this pressure point is activated due to the increased blood pressure in the thoracic aorta, it stimulates the vagus nerve, which will, in turn, reduce the heart rate.
Although it has been acknowledged by many experts to be very good for patients having supraventricular tachycardia, the success rate is highly variable and may depend on various factors.
Studies that have examined this maneuver have reported success rates of about 6 to 54%. This could be partly because the effectiveness of this procedure is also dependent on the patient as much as the doctor.
R
Roemheld Syndrome
By nature, Roemheld Syndrome is not a single disease but a syndrome, i.e., a combination of symptoms that occur simultaneously and are caused by one or more pathologies.
In a typical case, patients with Roemheld Syndrome suffer from gastrointestinal disease and present with arrhythmia or abnormal heart rate (tachycardia or bradycardia).
The exact etiology of RS is unknown, but studies suggest that the anatomical proximity of the heart to the GIT, vagus nerve (VN) stimulation and electrolyte deficiencies are possible causes of the cardiac symptoms, vagus nerve stimulation being the most widely suspected cause.
W
Wolf-Parkinson-White Syndrome
Wolff Parkinson White syndrome occurs with a frequency of 1-3 cases per 1000 people.
Specialists say that some people are born with an anatomically abnormal pathway that conducts electricity. It is present like a bridge between one of the atria and one of the ventricles and will conduct the impulse from atria to ventricles bypassing the atrioventricular node (AV).
The mechanism in WPW is that the impulse travels on both tracks, the normal conduction and the abnormal one, but much faster on the abnormal pathway because that cable of tissue is not designed to slow the conduction of impulse as an atrioventricular node (AV) does.