Have you ever been walking and, out of nowhere, you feel something strange happening in your chest? Like your heart is beating without a regular rhythm or you’re suddenly drowning? If this is the case and it has happened to you or a loved one, then pay attention, as it may be Ectopic Beats, one of the most common heart disorders.
Ectopic beats can be very uncomfortable for people aware of their symptoms but are usually not dangerous in healthy individuals with a structurally normal heart who only have isolated palpitations, which occurs in almost all patients. However, a frequency of over 10 000 ectopics/day may be problematic.
Some cases are often complicated by certain previous disorders, heart structural alteration, or associated risk factors, such as age and some cardiovascular conditions.
Table of Contents
What are Ectopic Beats?
Ectopics are abnormal heartbeats of an atrial or ventricular origin that alter that rhythm and cause a series of annoying symptoms.
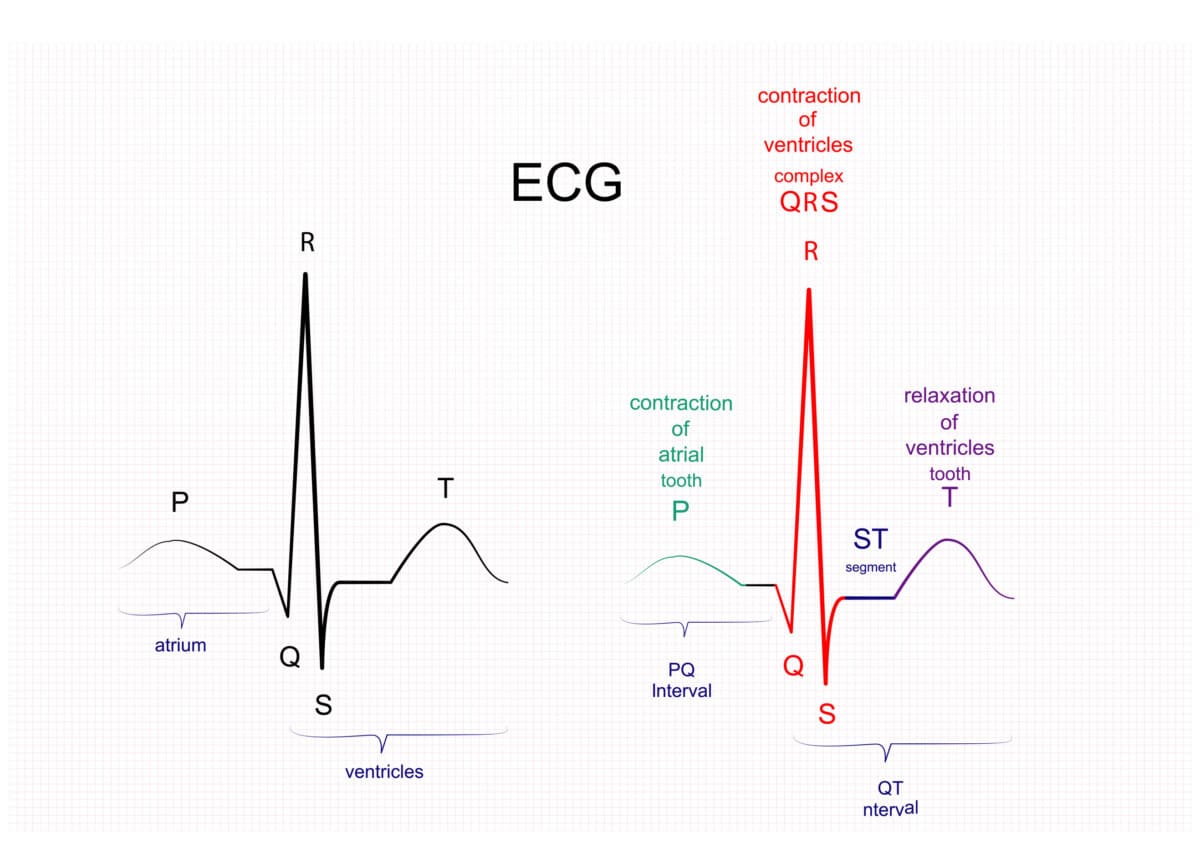
Before describing in detail an ectopic beat, we need to learn about the uniqueness of the cells inside the heart and what is the normal pathway of an electrical impulse.
The heart has its own regulatory system called the electrical conduction system which sets the heartbeat. This mechanism represents the build-in electrical system placed in the heart walls that allows the electricity to be generated and which coordinates the rhythm.
Electricity is the driving force behind every heartbeat. Our heart needs electricity to work.
Imagine like electrical wires that go from top to the bottom of the heart and transmit the current throughout the heart muscle.
At the cellular level, we have two types of cells in the walls of the heart:
- 99% contractile fibre, responsible for heart contraction, for pumping the blood
- 1% conducting fibre which spreads the electrical impulses throughout the heart. They are not nervous tissue, don’t contract but are formed to be electrically active.
The conduction fibres are autorhythmic which means they have the ability to generate spontaneous electrical impulses producing electricity on their own without neurological or hormonal input.
Their role is to generate and conduct current, cell to cell throughout the heart, stimulating the heart to contract and pump blood.
All cells from the heart muscle are capable of producing an electrical impulse, in other words, to create a heartbeat.
However, the impulse that controls the normal rhythm is carried out ONLY along with the components of the cardiac conduction system from two reasons:
- The SA node is faster in initiating the electricity than the other cells in the heart
- The cells in the cardiac conduction system are more specialised in conducting the impulse than any other cells
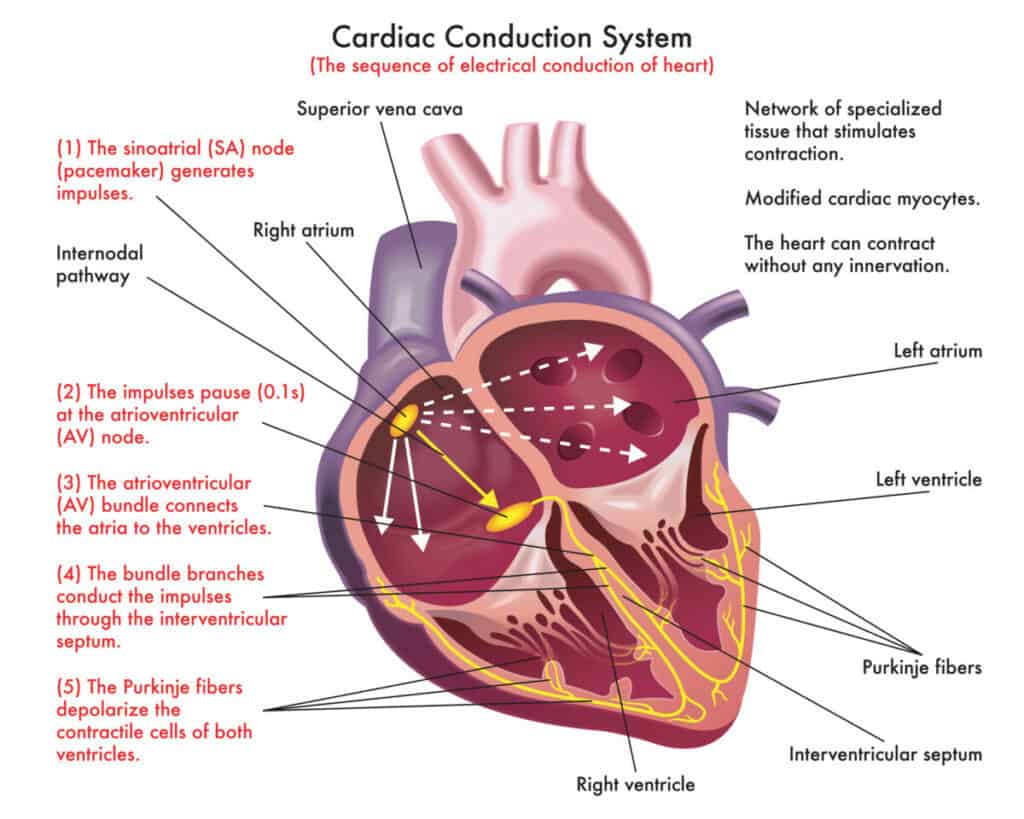
The electrical pathway of the heart consists of:
- Sinoatrial node (SA node)
- Atrioventricular node (AV node)
- Atrioventricular bundle or the bundle of His
- Bundle branched
- Purkinje fibres
In a normal heartbeat, the impulse is born in the sinoatrial node (SA node), passes through the atrioventricular node (AV node), then goes down to the bundle of His and Purkinje fibre until it reaches the last cell of the heart and feeds it with electrical energy, so that it can function and contract, thus allowing the heart to beat.
What is going on in my heart when having an ectopic beat?
There are many causes behind this disorder but the biggest problem is that our heart develops other “batteries” (pacemakers) that serve as the origin of the electrical impulse, generating several impulses that run through our heart at the same time.
Ectopic means misplaced or in abnormal place.
Ectopics are the early or additional heartbeats that can lead to the perception of palpitation. They arise from other regions than the SA node.
Under normal conditions, electrical impulses are under the control of the sinus node (SA node), which guides and suppresses them.
The problem is that other electrically active areas of the heart with dominant stimuli may appear.
Time to time one of the heart’s cells get irritable and decide to generate an ectopic beat.
While our original sinus node (SA node) tells the heart cells to contract and generate the heartbeat normally, there is another impulse, the ectopic, that tells them to do it again, when they are not even ready for it.
The sinus node can perceive this abnormal stimulus and delay the normal heartbeat a bit so that the heart can recover.
Furthermore, even though the ectopic beat has an electrical presence, the mechanical effect is weaker. Therefore it’s not doing much in terms of pumping the blood.
The symptoms arise from this interlocking of the beats. Because the ectopic beat is not effective, the next beat, coming from the sinus node is much stronger and must push the blood that was left into that beat, partially “drowning” the heart in its desperate attempt to expel everything.
Depending on the origin of this second electric impulse, we can differentiate two types of ectopic beats: premature atrial contraction (PAC) and ventricular premature contraction (PAC).
Premature Atrial Contraction (PAC)
The sinus node (SA node) is in the right atrium (one of the two upper chambers of the heart).
It is responsible for giving rise to our original impulse, creating the “sinus rhythm” (the normal rhythm of any healthy heart).
However, in some cases another impulse may be formed from another sector of the atrium (right or left), giving rise to an abnormal second heartbeat that may be before or after the typical heartbeat.
This is Premature Atrial Contraction where there is an early electrical impulse in the upper chambers of the heart called the atria.
If these happen, the ectopic beats will occur at the upper part of the heart.
The exact cause of this disturbance is not yet well known; however, several predisposing factors are worth mentioning. In addition, many of those who suffer from this disorder (such as older adults, where it is more common) do not have significant symptoms or require any further attention besides the normal follow up.
This type of ectopic beat is asymptomatic in almost all patients. Some have additional complications because they are usually older adults, so the symptoms can be confused. The only way to detect it is with a Holter monitor.
The risk factors related to PAC are
- Age (over 55)
- High BMI
- Previous cardiovascular disorders
- Altered lipid profile (high cholesterol)
- Abnormal Atrial Natriuretic Peptide
Ventricular Premature Contraction (PVC)
Unlike PAC, the early impulses originate in the lower chambers of the heart, known as the ventricles.
The latter is more frequent, and the electrical impulse is born in the final portion of the circuit, known as the Purkinje Fibers, and not in our natural pacemaker, the sinus node.
When having ectopic beats, we may feel symptoms due to the heart trying to compensate for the ectopic rhythms, or we may not even know that we have an ectopic rhythm.
Although it is not usually dangerous, in some cases, it can be prolonged or complicated by other cardiac arrhythmias, giving it a particular character of importance.
All arrhythmias have about a 20% chance of combining with other cardiovascular disorders, which is usually a problem.
However, in the case of PVC (also known as ventricular extrasystole), by itself, it does not pose any significant risks. It is essential to mention that this is the cause of the symptoms related to ectopic beats (although it can manifest itself without symptoms). Among these we have:
- Chest pain
- Faint feeling
- Hyperventilation
- Drowning
- Weakness
- Palpitations (strong beats)
- “Missing” beats
Differences between PAC and PVC
- Do they feel the same? PAC is usually asymptomatic; the only way it can show symptoms is if another arrhythmia accompanies it. Therefore, if you feel dizziness, sudden hyperventilation, chest pain or strong beats, it is most likely a PVC.
- Which one is more dangerous? The PVC. However, the risk is very low and is associated with prolonged symptoms and other added risk factors (such as basal cardiovascular disease). Many people lead normal lives without even knowing that they have PVC.
- How do I know if my ectopics are PVCs or PACs? The only way to confirm the information is with a pacing holter, a study where a small portable heart monitor is placed on your arm or neck, with a series of electrodes that continuously record the electrical information of your heart, usually over 24 hours. This is a test indicated only by a cardiologist or a related specialist.
Are Ectopic Beats Dangerous?
As I said earlier, ectopics have very annoying manifestations. Still, they are not dangerous if after doing the tests and investigation required by your doctor, it turns out that your heart is healthy.
However, ectopic heartbeats are dangerous under certain conditions. These are three crucial points for identifying dangerous ectopic beats:
Quantity: How many PVCs are too many?
The number of times during the day that ectopic beats appear is essential.
It is not the same if it is only once, totally isolated to another event and without major symptomatic complications, as if it were thousands and repetitive.
Having ectopic heart rates of over 10000/day are dangerous. Why? Because in time, the heart becomes weaker, less blood is going around the body and to the heart, and as a result, we have symptoms like fatigue and tiredness.
With an ectopic beat, the heart pumps faster and remember, the heart is a muscle and can get tired and overworked just like any other muscle in your body.
Just because the heart is a unique muscle that pumps blood 24 hours every single day for as long as we live does not mean it cannot get tired.
We do not have to worry about our hearts getting “tired” if it is pumping blood at the normal rate, but at abnormal rates, a lot of things could go wrong.
Of course, our bodies know that the heart must continue pumping blood no matter what. So what the heart does when it is “tired” is that it tries to compensate. But, after a while that fails and we begin to see issues like cardiac arrest, cardiomyopathy, chronic heart failure etc.
Studies do show that a high number of PVCs in a long period may induce disease of the heart muscles.
The definition of high-frequency PVCs can vary from 10,000 to 20,000 PVCs/day
study on the effect of premature ventricular complex burden on long-term outcome
Studies have shown a consistent link between premature ventricular contraction and left ventricular hypertrophy, especially in hypertensive people.
This is just a fancy word for bigger ventricle (lower chamber of the heart) muscle. This makes sense because just like our muscles get bigger when we work out, so does the heart muscle.
Ectopic beats make the heart muscle work more coupled with the fact that there is increased resistance in the blood vessels of those who have hypertension and the left ventricles pump blood to the body.
It is like making the heart “work-out”. The results are bigger muscles in left ventricles. This is not a good sign as it has been linked to increased chances of heart attack and chronic heart failure.
You must go to a specialist to quantify or even to confirm the presence of ectopic beats which is done by wearing a Holter monitor. The 24-hour record will show how many times a day you suffer from ectopic beats.
Structural alteration
The condition of your heart is crucial. For example, left ventricular and atrial hypertrophy, which is common in essential hypertension, can be a trigger for the onset of heart rhythm disorders.
Also, some pathologies can affect other sectors of our cardiovascular system and have the same impact on our heart.
How do I know if my heart is OK?
The best and most direct method is the echocardiogram, which uses ultrasound to obtain images of your heart and the adjacent structures, allowing us to carefully analyze each area in the search for functional or structural alterations. In the echocardiogram, we can even observe the speed and type of flow through your heart.
Triggers
Another critical point is the conditions, foods, or objects that you have determined to be exacerbating your heart disorder. Some things can aggravate an ectopic beat such as electrolyte imbalance, heart disease, smoking alcohol, caffeine and some over the counter drugs. It is better to avoid these if you are prone to ectopic beats.
Some people tend to be more reactive to physical activity, although there is also literature that mentions some foods such as chocolate and coffee. However, it is necessary to emphasize physical activity since it is one of the most common triggers.
When you usually have these ectopic beats – at rest or when you exercise?
Ectopic beats don’t present a risk in all people who are experiencing them while exercising. However, you should be concerned if you exercise regularly and have ectopic beats every time. But if you experience them only from time to time and they don’t get worse with continuing exercise, they are most likely benign and nothing to worry about.
If you have consistent and progressive ectopic beats seen as palpitations or skipped beats when exercising it might show that you have myocardial ischemia. Myocardial ischemia is another fancy medical term to describe when your heart muscle is not getting enough blood and hence enough oxygen.
The easiest way is to do an exercise stress test, which subjects the patient to some basic physical effort (such as running on a treadmill for a few minutes) while connected to a heart monitor, which records the activity of his heart.
How to get rid of ectopics?
The only way to get rid of ectopic beats is to know their cause. Most of these disorders have a recognizable origin that is not limited to structural disturbances (such as atrial or ventricular hypertrophy), but almost any functional disease can cause ectopic beats. Here is a list of possible causes and triggers:
- Lifestyle Triggers: Some basic things in our lives can cause palpitations. These include exercise, lack of sleep, alcohol, smoking, caffeine, and even some spicy foods.
- Emotional or Psychological: Changes in our behaviour due to external situations can cause palpitations, such as excitement or nervousness. However, psychiatric disorders are also included in this group (stress, anxiety, panic attacks, etc.)
- Structural or functional alterations: it may be that it is cured with some added cardiovascular disorder that caused the ectopic beats. In addition to hypertrophy (atrial or ventricular), there may also be electrical problems (creation of new pacemaker sites), etc.
- Non-cardiac disorders: Almost any alteration in your body, be it metabolic or structural, can trigger the appearance of ectopic beats.
Each person may have a disorder that causes the appearance of or triggers ectopic beats. Therefore, everyone needs a personalized evaluation with an individual plan for treatment and symptom control based on a cause that must be identified. There is no magic cure that can eliminate the problem forever; each case needs to be diagnosed and treated separately.