Supraventricular tachycardias (SVTs) are common in both children and adults and so far, despite thousands of hypotheses about their cause, we know nothing concrete.
However, many experts have determined certain markers that could be indicators of the development of these cardiac arrhythmias. But can chronic inflammation be the cause of SVT?
Inflammation comes from the root inflame, from the Latin word inflammare meaning “to set on fire.”
www.vocabulary.com
Interviewing two medical doctors and analyzing scientific studies helped to conclude that chronic inflammatory reactions are linked to the development and establishment of SVT. According to the studies, the elevation of the Neutrophil/Lymphocyte ratio, which represents an inflammatory marker, predicts the appearance of SVT.
These findings could be the start of further research to help us understand how this disease originates and, therefore, how to treat it appropriately. So far, there are only invasive therapies and symptom-preventive control in allopathic medicine, nothing that will really “cure” completely or prevent the recurrence of these disorders.
I interviewed Dr. Andres Davidv and Dr. Okoli Chukwuebuka to learn more about the relationship between chronic inflammation and heart health.
Dr. Okoli Chukwuebuka a Nigerian-born doctor, he’s 27 and is currently doing his residency program in internal medicine at Abia state university’s teaching hospital in Aba, Nigeria.
Dr. Andrés Velásquez earned his MD with the honorific mention (Cumlaude) from the Universidad de Oriente, a top medical school in Venezuela. He is an Internal Medicine Resident at the Hospital “Herminda Martin” and Clinical Manager of the Home Care Pharmacy Committee in Venezuela.
In the interview I have addressed the following questions:
- Can chronic inflammation be the cause of SVT?
- How to test for chronic inflammation?
- Can we have chronic inflammation with normal blood tests?
- What does chronic inflammation do to the heart?
- What are three things that protect our heart against inflammation?
Table of Contents
Doctors’ Opinion About Chronic Inflammation Link To SVT
Supraventricular tachycardia could be considered a type of arrhythmia where there is a fast heartbeat. SVT is an alteration of the normal heart rhythm due to the deterioration of the cardiac cells’ electrical connections. It may appear abruptly or progressively when it is associated with an acute condition.
1. Can Chronic Inflammation Be The Cause Of SVT?
g
Dr. Andrés Velásquez‘ Response:
Of course, chronic inflammation has been shown in pediatric patients with supraventricular tachycardia (SVT). These patients generally present two important peaks in SVT development, during early childhood and between the eighth and twelfth year of life.
In these patients, high levels of some inflammatory markers (neutrophils and lymphocytes) have been evidenced that could be closely related to the development of supraventricular tachycardia.
When inflammatory processes exist, the immune system deploys its cellular components to fulfill its protective functions. It is important to mention that these patients did not present another organ/system infection or some other associated pathology.
g
Dr. Okoli Chukwuebuka‘s Response:
Yes, there could be some relationship between chronic inflammation and SVT.
Though research is still ongoing about this, it has not been proven whether the SVT itself results from the inflammatory process or whether they just co-exist. Placing patients with SVT on anti-inflammatory medications such as Steroids and NSAIDs can aid in the recovery process, especially post-operatively, is a piece of reasonable evidence to consider. New drugs with both anti-inflammatory and anti-arrhythmic action might be beneficial in this case.
g
Reflection: The consensus is that there is a link between chronic inflammation and SVT. One suggestion was that more studies in this area are needed to bring some light to this problem and see if inflammation is the cause of SVT or if the two coexist. There is a large amount of scientific evidence showing that chronic inflammation is behind almost every disease. I think we can say with some certainty that SVT can fall into this group of diseases due to chronic inflammation.
2. How To Test For Chronic Inflammation?
g
Dr. Andrés Velásquez‘ Response:
Currently, the tests mostly used in the clinical practice to diagnose inflammatory states are C-reactive protein (CRP) and Erythrocyte sedimentation rate (ESR).
The C-reactive protein (CRP) is a protein that manifests itself in the acute phase of inflammation and functions as an inflammatory marker of tissue damage. This protein modulates the intensity and area of extension of inflammation in the acute phase. CRP is synthesized in the liver and sent to the blood when infection, tissue damage, and acute or chronic inflammation occur in the body.
Erythrocyte sedimentation rate (ESR), a method that expresses the acute-phase inflammatory response. It is the speed at which red blood cells precipitate in a period of one hour in a blood sample. Normally, red blood cells stabilize relatively slowly. A faster than normal rate may indicate the presence of inflammation in the body.
g
Dr.Okoli Chukwuebuka‘s Response:
One of the tests for Chronic inflammation is the Serum Protein Electrophoresis (SPE). This test measures the amount of certain proteins in the blood that reflects an inflammatory state.
The most important being the C-reactive protein (CRP), CRP values between 10mg/l – 100mg/l are considered to be within the inflammatory range, but values above 100mg/l indicate a severe bacterial infection.
Another test is the Erythrocyte Sedimentation Rate (ESR). This test measures how fast RBCs settle in a tube containing blood. The faster they get to the bottom of the tube, the more likely inflammation exists.
g
Reflection: These are tests currently used in clinical practice and can be requested from your family doctor. They help to establish the diagnosis and monitor the evolution of certain diseases. The most common tests to measure inflammation are Serum Protein Electrophoresis (SPE), C-reactive protein (CRP), and Erythrocyte Sedimentation Rate (ESR).
3. Can We Have Chronic Inflammation With Normal Blood Tests?
g
Dr. Andrés Velásquez‘ Response:
Yes, normally, CRP values below 10 mg are considered within normal limits. Despite this, we can have a mild inflammatory process within normal values. The inflammation is persistent but in low intensity.
Higher CRP values suggest a more severe inflammatory process, with greater probabilities of manifesting symptoms, since the greater the degree and extension of the inflammatory process, the greater the affection to systemic organs.
For example, in a patient who has rheumatoid arthritis, an autoimmune pathology with an inflammatory component, doctors can evaluate the current risk according to the reported levels and the degree of inflammation through the PCR test.
g
Dr. Okoli, what’s your take on subclinical inflammation?
Dr.Okoli Chukwuebuka‘s Response:
Subclinical inflammation is a low-grade inflammatory response that may have no symptoms at first and occurs due to an alteration in the normal levels of immune mediators in the body like pro-inflammatory cytokines such as IL-6 and TNF-a or anti-inflammatory cytokines such as IL -4 and IL – 10.
Pro-inflammatory cytokines contribute by enhancing and stimulating the inflammatory response, while anti-inflammatory cytokines reduce the inflammatory response. So when there’s an imbalance between these mediators, inflammation occurs.
This low-grade inflammation is a result of the prolonged presence of these pro-inflammatory mediators after fighting off a foreign body or an infection, instead of reducing in numbers they accumulate and this can cause them to form plaques leading to continued inflammatory responses.
Chronic (low-grade) inflammation can occur in the arteries, liver, brain, muscles, and joints leading to several diseases including heart disease, stroke, diabetes, arthritis, depression, and even cancer.
Some factors that contribute to this low-grade inflammation include obesity, genetics, unregulated stress, smoking, excessive alcohol intake, lack of exercise, poor diet, and increasing age.
g
Reflection: The previous question aimed to identify tests that detect inflammation in the body. However, if these tests result are within normal limits, but I do not feel well, and I have symptoms that cause me discomfort, I must also consider the possibility of subclinical inflammation.
4. What Does Chronic Inflammation Do To The Heart?
g
Dr. Andrés Velásquez‘ Response:
Inflammatory processes promote atherosclerosis by attracting cholesterol (LDL), which undergoes an oxidation process in the wall of the blood vessels. The blood vessel walls thicken due to the accumulation of atheroma plaques or lipids. It leads to the accelerated evolution of coronary disease that eventually shows pump failure if not controlled. In chronic inflammatory processes, this inflammatory influx is permanent, promoting the obstruction of blood vessels much faster than in an average patient.
g
Dr.Okoli Chukwuebuka‘s Response:
Starting with stress, be it physical, mental, or emotional, can cause an increase in heart rate, ultimately leading to increased blood pressure.
Obesity can affect the heart structurally and functionally leading to arrhythmias and also excess cholesterol in the body can lead to atherosclerosis (fat plaques blocking blood vessels) this can lead to inadequate blood supply to and from the heart and can also lead to coronary artery disease.
Smoking, obesity, stress, and all the factors that I have already mentioned have a detrimental effect on the heart causing various illnesses, including cardiovascular diseases.
g
Reflection: Risk factors such as stress, lack of physical activity, poor diet, smoking, and high cholesterol have a significant role in maintaining chronic inflammation and developing cardiovascular disease.
5. What are three things that protect our heart against inflammation?
g
Dr. Andrés Velásquez‘ Response:
The three most important actions that we must consider to protect our heart from chronic inflammatory processes are: maintaining a balanced diet, avoiding the consumption of excessive fats and foods that are naturally inflammatory, physical exercise, and managing stress.
Exercise should be perceived as a lifestyle. And stress should be avoided at all costs since the amount of pro-inflammatory substances triggered by stress and depression has been shown. If the patient suffers from hyperlipidemia, other drugs could be associated to avoid future complications, depending on the clinical case.
g
Dr.Okoli Chukwuebuka‘s Response:
The three most important things somebody can do to protect her or his heart against chronic inflammation are diet modifications, lifestyle modifications, and medication.
We should adjust our food intake and diet, eating less fatty foods, and incorporate food items such as fish oil, ginger, garlic into our meals. Also, we should try and control our blood sugar levels by taking less of sugar-containing foods.
We should exercise regularly to burn excess fat, lose cholesterol, and keep the heart pumping efficiently and effectively.
Non-Steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil) or Naproxen (Aleve) can help reduce inflammation. Also, Steroids such as corticosterone can help to reduce inflammatory responses.
g
Reflection: No one can deny the importance of lifestyle in preventing chronic diseases, especially heart disease. Two out of the three things recommended by both interviewed doctors to prevent chronic inflammation are lifestyle changes and exercise. Anti-inflammatory medication has also been mentioned to reduce inflammation. Still, I want to say that its adverse effects have a spectrum of action on the whole body, interact with other drugs, and are not recommended for pregnant women.
Does Chronic Inflammation Cause SVT? (what studies show)
To explore this possibility further, several experts decided to investigate the different parameters and markers that could be used to test this theory.
The neutrophil/lymphocite ratio (NLR), was set to evaluate the magnitude of the inflammatory processes and the prognosis of patients just out of surgery.
Since its discovery, it has been used to predict and study the mechanism and development of various diseases, from the mildest to the most severe (such as colon cancer). Some medical researchers decided to use it for SVT, due to hypotheses raised that chronic inflammation may be at the origin of this disorder.
Although many studies have shown direct and quite conclusive results, I would like to highlight two of them, which have quite amazing evidence.
SVT in older patients (1)

In 2016, Dr. Mesut Aydin from Dicle University, Turkey, supervised a study conducted to better understand the correlation of neutrophil/lymphocyte ratio (NLR) and supraventricular tachycardias (SVTs).
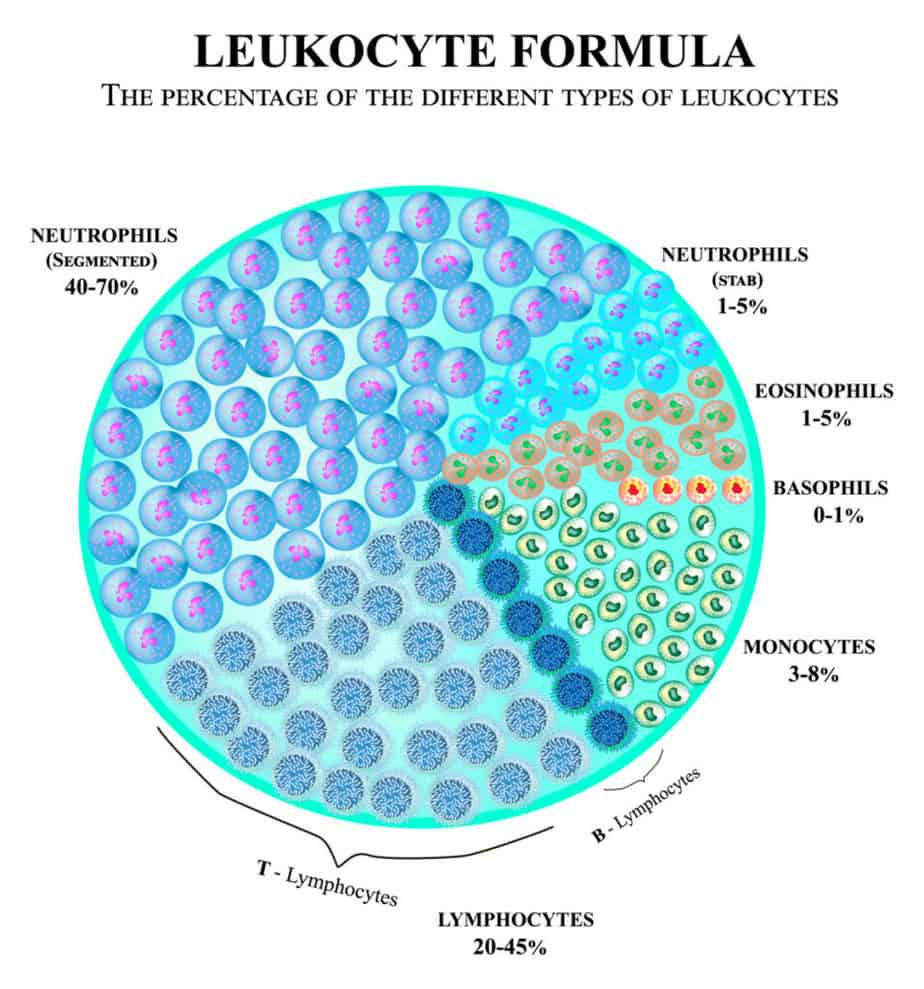
Neutrophils represent 50 – 70% of white blood cells. They are the first sent to detect and act if an infection is present in the body.
Lymphocyte represents 20 – 30% of white blood cells and they have a complex role in attacking and destroying foreign cells.
Previously, little to no significant research was present on this topic, which created a void. The study was expected to fill the gap and evaluate the relationship between the ratio of different immune cells and the abnormal heartbeat.
Statistical data used in this study was collected from 150 SVT patients and 98 healthy controls. Of the 150 patients selected, 90 presented AV-nodal reentrant tachycardia, 37 presented Wolff-Parkinson-White syndrome and 5 atrial tachycardia. These patients presented no chronic diseases.
Electrophysical study (EPS) was performed in patients with a pre-diagnosis of SVT.
Electrophysical study is a test conducted to access the electrical system of the heart and helps to identify any abnormal heartbeats or arrhythmia.
Patients in which arrhythmia focus was detected, underwent radiofrequency ablation (RFA) therapy.
Ablation procedure uses radio waves to heat and destroy the abnormal cardiac cells responsible for arrhythmia.
Blood tests were used to compare the hematological parameters. The neutrophil count was higher, while the leucocyte count was lower in the SVT patients than in the control group.
This demonstrated significantly higher neutrophil/lymphocyte ratio values in the SVT group when compared to the healthy subset of people. More than 67% of patients with SVT developed a higher than usual NLR.
The group of 150 SVT patients was further divided into two separate subgroups depending on whether EPS induced tachycardia or not. Patients who experienced elevated heartbeat as a result of EPS also showed higher NLR readings than those who didn’t suffer from induced tachycardia.
The study observed significantly higher neutrophil/lymphocyte ratio (NLR) readings in patients suffering from SVT than in the control group.
Hence, the study statistically established a notable correlation between high NLR values and SVT cases.
SVT during the first year of life – could inflammation be the trigger? (2)

Similar conclusions were reached in an article by Pier Paolo Bassareo et al (2016)2 titled “Supraventricular tachycardia during the first year of life: is subclinical inflammation the trigger?
A number of 18 newborns diagnosed with SVT but with no other illnesses were selected for the study. The control group included 18 healthy newborns.
After running the tests and comparing the results, the experts determined that the elevation of the NLR was clearly involved in the development of SVT.
They even ruled that there is a direct link that would make it possible to predict and quantify each patient’s risk of suffering this pathology.
The reason is that there is a demonstrable chronic inflammatory disorder with the NLR, where the lymphocytes are elevated, altering that relationship.
Based on the results of this study, we could determine the risk, presence, and absence of SVT in pediatric populations with a simple neutrophil/lymphocyte ratio (NLR). We would not even need an electrocardiogram, but only with a blood sample would we have a clear and concise answer in a short time.
What is inflammation?
Although we know how SVT works and the mechanisms that trigger the electrical disturbance with each heartbeat, we still don’t know what causes it. We have not discovered what is the basic disturbance that causes this defect in the atria.
What we do know is that there are several factors that can act as indicators or predict the onset of SVT. One of these is chronic inflammation, a prolonged reaction of our immune system characterized by a severe cellular response, where there is continuous tissue damage and a permanent attempt by our body to repair it.
How inflammation manifests in our body?
Acute inflammation
When you badly scratch your hand, an acute inflammatory process immediately begins on that affected area.
The blood flow increases because the immune system will send to the wound a large number of specific small blood cells called platelets. These cells will stick together and form a kind of wall that stops the bleeding.
Then the leukocytes, a type of white cells, are sent to eliminate any bacteria present in the wound.
Macrophages which are large white cells, will continue the cleansing process and help develop new cells.
That tissue will be sore, red, and a little bit swollen. In three or four days, the inflammation is gone and begins the phase of regeneration and healing of the tissue. This is how acute inflammation works.
If the inflammation had not occurred, the wound would not have healed, and a possible infection could not have been controlled.
The initial inflammation that occurs after an injury is a normal response of the immune system to protect our health.
Chronic inflammation
Let’s say you have been eating for years a Standard American Diet with many processed foods, sweets, sugary drinks, a high intake of red meat, pre-packed meals, and pastries. Toxins such as cigarette smoke, alcohol, pesticides, contaminants from your tap water, parabens from cosmetics also influence your health.
Your immune system is now struggling to detox and neutralize all those toxins. When your body is not treated well because of these agents, your immune system will come into rescue the same way how it did to the scratch on your hand.
All these agents act on the body every day and the inflammatory process becomes continuous.
It’s like scratching your hand in the same place all the time.
Acute inflammation has the role of repairing the tissue while chronic inflammation can grow and spread slowly for a long time wearing down the whole body.
Chronic inflammation is behind many disabling diseases in humans. Some that we can mention are autoimmune diseases, allergies, rheumatoid arthritis, atherosclerosis, tuberculosis, and pulmonary fibrosis.
Some practitioners say that inflammation is behind every chronic illness. It is a clinical process, clearly observed by doctors through tests and investigations or subclinical when despite investigations done, nothing is found.

Final Thoughts
Supraventricular Tachycardia (SVT) is a heart rhythm disorder that poses a risk for sufferers. Despite thousands of investigations and studies, we still do not know why it occurs. However, several factors could guide us to prevent the possible development of this pathology. One of them, and perhaps the most important, is undoubtedly the presence of inflammation reflected by the high value of the NLR ratio, as we have determined with the studies cited above.
Exploring the possibility that chronic inflammation is the cause of SVT could change the diagnosis and treatment of SVT, facilitate doctors’ work, and improve the quality of life of patients suffering from this disease.
| Inflammation | Acute | Chronic |
| Result | Helps in the process of healing | Does not bring healing. It contributes to the development of other diseases |
| Duration | Lasts several days | Lasts months or years |
| Finding | It is localized | It affects the whole body |
| Causes | A wound, a sore throat, a sprained ankle | Chronic diseases, repeated acute inflammation, external or internal stressors |
| Symptoms | Pain, redness, stiffness, swelling, heat | Pain, chronic fatigue, fever, or no symptoms |
Disclaimer: The information on this blog post is not intended to diagnose, cure, or treat any disease. I don’t provide medical advice. I only share my health transformation journey and what I have learned along the way. This site is meant for informational purposes only. Please consult your doctor before applying any information from this blog.

